Liver Cancer: Causes, Symptoms, Diagnosis, Prevention, and Treatment
Introduction
Liver cancer is a life-threatening disease that originates in the liver — one of the most vital organs responsible for detoxification, metabolism, and nutrient storage. The global burden of liver cancer is increasing, especially in regions with high rates of hepatitis infections and alcohol consumption. Despite being a serious condition, early diagnosis and modern treatments have significantly improved survival rates.
In this comprehensive article, we will explore what liver cancer is, its causes, signs and symptoms, diagnostic procedures, prevention strategies, and available treatment options.
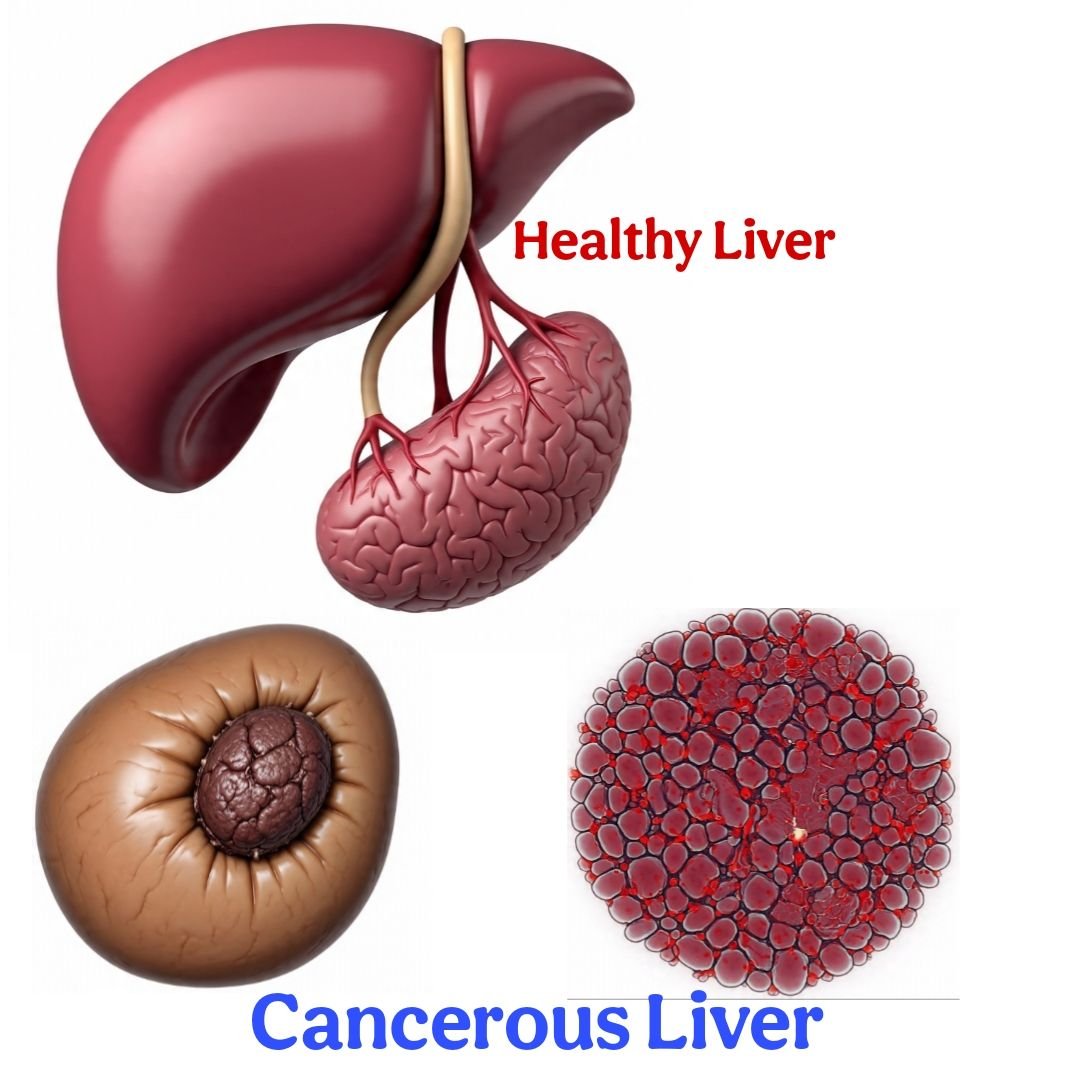
What Is Liver Cancer?
Liver cancer, also known as hepatic cancer, refers to cancer that starts in the liver. It can be classified into two main categories:
• Primary liver cancer: Begins in the liver cells.
• Secondary (metastatic) liver cancer: Spreads to the liver from another part of the body.
The most common type of primary liver cancer is hepatocellular carcinoma (HCC), accounting for about 75% of all cases. Other types include cholangiocarcinoma (bile duct cancer), angiosarcoma, and hepatoblastoma (more common in children).
Causes and Risk Factors of Liver Cancer
Liver cancer often develops due to long-term liver damage or chronic liver diseases. Major risk factors include:
1. Chronic Hepatitis B or C Infection
Long-term infections with Hepatitis B Virus (HBV) or Hepatitis C Virus (HCV) are the leading causes of liver cancer. These infections can lead to cirrhosis, a major predisposing factor.
2. Cirrhosis
Cirrhosis is scarring of the liver tissue, which severely impacts liver function and increases cancer risk. Causes of cirrhosis include:
Alcohol abuse
Nonalcoholic fatty liver disease (NAFLD)
• Viral hepatitis
• Autoimmune liver diseases
3. Alcohol Consumption
Heavy alcohol use over several years can lead to cirrhosis, thereby raising the chances of liver cancer.
4. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD, often associated with obesity, diabetes, and metabolic syndrome, is an emerging cause of liver cancer worldwide.
5. Aflatoxin Exposure
Aflatoxins are carcinogens produced by molds that grow on stored grains and nuts. Ingestion over time increases liver cancer risk.
6. Genetic Disorders
Inherited diseases like hemochromatosis (iron overload) and Wilson’s disease (copper overload) can damage the liver and lead to cancer.
7. Diabetes and Obesity
People with diabetes and excess body weight are at increased risk of liver cancer, especially if associated with fatty liver disease.
8. Smoking
Tobacco use contributes to liver cancer risk, especially in combination with other risk factors.
Signs and Symptoms of Liver Cancer
Liver cancer often goes undetected in the early stages because it may not cause noticeable symptoms. As the disease progresses, symptoms may include:
Early Symptoms:
• Fatigue
• Loss of appetite
• Unexplained weight loss
• Abdominal discomfort or fullness
• Nausea or vomiting
Advanced Symptoms:
• Pain in the upper right abdomen
• Swelling in the abdomen
• Yellowing of the skin and eyes (jaundice)
• Enlarged liver or spleen
• Dark-colored urine
• Itchy skin
• Fever
If any of these symptoms persist, especially in individuals with known liver disease or risk factors, medical attention is essential.
Diagnosis of Liver Cancer
Early detection of liver cancer can improve treatment outcomes significantly. Diagnostic procedures include:
1. Physical Examination
A doctor may feel the abdomen for lumps or swelling and evaluate other signs like jaundice or weight loss.
2. Blood Tests
• Alpha-fetoprotein (AFP): High levels may indicate liver cancer.
• Liver function tests (LFTs): Assess overall liver health.
3. Imaging Studies
• Ultrasound: Often the first imaging test used.
• CT Scan (Computed Tomography): Provides detailed cross-sectional images.
• MRI (Magnetic Resonance Imaging): Helps differentiate benign from malignant tumors.
4. Liver Biopsy
A sample of liver tissue is collected and examined under a microscope to confirm cancer.
5. Liver Elastography or FibroScan
These tests help assess the degree of liver fibrosis or cirrhosis.
6. Staging
Once liver cancer is diagnosed, it’s essential to determine its stage to decide on appropriate treatment. Staging involves checking tumor size, lymph node involvement, and metastasis.
Prevention of Liver Cancer
While some risk factors like genetics cannot be modified, many preventive steps can significantly reduce the risk of liver cancer:
1. Vaccination Against Hepatitis B
A safe and effective vaccine is available to prevent HBV infection, reducing the risk of liver cancer.
2. Control of Hepatitis C
No vaccine exists for HCV, but antiviral medications can cure most cases, thus lowering cancer risk.
3. Avoid Excessive Alcohol
Limiting alcohol intake protects the liver and reduces the risk of cirrhosis and liver cancer.
4. Maintain a Healthy Weight
Obesity and fatty liver disease are risk factors. A balanced diet and exercise can help reduce the risk.
5. Healthy Diet
Avoid foods contaminated with aflatoxins (like moldy grains and peanuts), eat antioxidant-rich fruits and vegetables, and limit processed food intake.
6. Regular Screening for High-Risk Individuals
People with chronic liver disease, hepatitis, or cirrhosis should undergo regular screening (ultrasound and AFP test every 6 months).
7. Avoid Smoking
Tobacco increases the risk of several cancers, including liver cancer.
Treatment Options for Liver Cancer
The treatment of liver cancer depends on factors like cancer stage, liver function, patient’s overall health, and whether the tumor can be removed. Major treatment options include:
1. Surgical Treatments
a. Liver Resection (Hepatectomy)
• Removal of the tumor-bearing portion of the liver.
• Suitable for patients with good liver function and a small tumor.
b. Liver Transplantation
• Recommended for patients with small tumors and poor liver function.
• Both the cancer and underlying liver disease are treated.
2. Ablation Therapies
a. Radiofrequency Ablation (RFA)
Uses high-energy radio waves to heat and destroy cancer cells.
b. Microwave Ablation
Similar to RFA but uses microwaves for faster treatment.
c. Cryoablation
Destroys tumors using extreme cold.
3. Embolization Therapies
a. Transarterial Chemoembolization (TACE)
Delivers chemotherapy directly to the liver tumor and blocks its blood supply.
b. Transarterial Radioembolization (TARE)
Uses radioactive beads to deliver internal radiation directly to tumors.
4. Targeted Therapy
Drugs like sorafenib and lenvatinib target specific pathways that cancer cells use to grow. These are used in advanced liver cancer cases.
5. Immunotherapy
Checkpoint inhibitors like nivolumab and atezolizumab help the immune system recognize and destroy cancer cells.
6. Radiation Therapy
While not commonly used due to the liver’s sensitivity, advanced techniques like stereotactic body radiation therapy (SBRT) can treat inoperable tumors.
7. Chemotherapy
Less commonly used due to limited effectiveness in liver cancer, systemic chemotherapy may still be considered in some advanced cases.
Prognosis and Survival Rates
Survival rates depend on the stage at diagnosis, liver function, and available treatments. According to cancer research data:
• The 5-year survival rate for localized liver cancer is about 35%.
• For regional spread, the rate is about 12%.
• For distant metastasis, it drops to around 3%.
• Early detection and treatment significantly improve outcomes.
Living with Liver Cancer
Managing liver cancer involves more than just medical treatment. Key aspects include:
• Nutrition: High-protein, liver-friendly diets help maintain strength.
• Support groups: Emotional and psychological support is vital.
• Regular follow-ups: Monitor for recurrence or side effects.
• Palliative care: Helps improve quality of life in advanced stages.
Frequently Asked Questions (FAQs)
1. Can liver cancer be cured?
Yes, if detected early and treated with surgery or liver transplantation. However, advanced cases are more difficult to cure but can be managed.
2. What is the most common symptom of liver cancer?
Unexplained weight loss, abdominal pain, and jaundice are commonly reported symptoms.
3. Who should get screened for liver cancer?
People with hepatitis B or C, cirrhosis, or a family history of liver cancer should undergo regular screening.
4. Is liver cancer hereditary?
Liver cancer is not usually inherited, but some genetic conditions can increase the risk.
5. Can lifestyle changes help prevent liver cancer?
Yes. Maintaining a healthy weight, avoiding alcohol and smoking, getting vaccinated against hepatitis B, and managing chronic liver diseases can reduce the risk.
Conclusion
Liver cancer is a serious condition that can develop silently and progress rapidly. However, with advances in early detection, preventive strategies, and personalized treatments, patients have better chances of survival and improved quality of life. Public awareness, vaccination, healthy lifestyle habits, and regular screenings are crucial in reducing the global burden of liver cancer.
If you or someone you know is at risk, speak to a healthcare professional about regular check-ups and preventive measures. Early action can save lives.
I hope that you liked this article.
Thanks!! 🙏 😊
Writer: Vandita Singh, Lucknow (GS India Nursing Group)